Healthcare May Indeed Be an Early Adopter for AI
The early signs of success from players in the space are promising, suggesting that the healthcare ecosystem’s ears are more open than one might think.
We like Hunter Walk’s line that “Your Thesis Is Your Portfolio Page, Everything Else is Just Hopes and Dreams.” When we say that we believe in the transformative power of technology in healthcare, we walk the walk:
Brightree* and ClearCare* in home health
Redox* and Machinify* in healthcare data
Continuum Cloud* and Modern Health* in behavioral health
Reify Health* in clinical trials
WebPT* in physical therapy
Curve Dental* in… guess 😊
Given our focus on the next generation of AI (previously written about here and here), healthcare was a natural starting point for us.
Despite healthcare's reputation for being risk-averse, our research shows a surprisingly proactive attitude toward AI adoption in this sector. This willingness is primarily fueled by the sector's administrative challenges, the costs of which now make up ~34% of total health care expenditures in the United States.
To understand this administrative resource drain more deeply, let’s explore three major culprits: clinical documentation, medical coding and prior authorization, all ripe targets for AI technology.
Clinical Documentation
Clinical documentation serves as the evidentiary record of patient visits, capturing critical data in real-time for integration into electronic health records (EHRs). This documentation becomes a central source of truth for treatment plans, coordination of care, medical coding and billing.
Today, healthcare providers rely heavily on human medical scribes, an expensive and error-prone approach, for completing substantial parts of this documentation. This outsourcing helps clinicians focus more on patients and less on taking notes, but comes at a significant cost: the global medical transcription market is expected to grow at a CAGR of 17.1% from 2022 to 2028 to reach a market size of $5.1B.
Even with all that expense, physicians still spend 2 hours per day on average completing clinical documentation outside of office hours. This contributes to the nearly 63% of physicians that report burnout in the US. And outsourced human scribes are not a panacea: even at the cost of up to $50k/year per scribe, the fast-paced clinical environment means that human scribes are not immune to human error.
The key question is when automated transcription will exceed human scribe performance and becomes industry standard.
Studies comparing human scribe error rates vs. automated transcription are sparse, from what we can tell — this one from JAMA Network in 2018 found that speech recognition software had error rate of more than 7% — but we see early signs that advancements in large language models are closing this gap. These new models make it possible for modern vendors to better understand the medical context of the conversations happening between doctors and patients and accurately structure contextually relevant information into the EHR.
This not only saves health systems money, but ultimately will improve the patient experience by allowing physicians to focus more on managing care plans and less on managing and monitoring scribes.
AI-enhanced documentation not only serves as a reliable source of truth but also streamlines downstream processes like medical coding and prior authorization.
Medical Coding
Once clinical documentation is completed, the notes are sent to a medical coder who translates the patient’s medical chart into a multi-digit alphanumeric medical code. This code is included as part of the claim that is sent to an insurance company for payment.
Navigating through a labyrinth of over 10,000 CPT codes and 68,000 ICD codes, coders can spend a few minutes to up to two exhausting hours generating just one accurate code, depending on the complexity and length of patient care. If the incorrect code is chosen, there are significant risks including lost revenue, legal investigations and potential exclusion from government-sanctioned programs such as Medicaid and Medicare.
The average claim denial rate is up 23% since 2016, and today, more than one in ten claims are denied at initial submission. While 63% of all denials in medical coding are recoverable, the costs associated with claim re-processing, payment and reconciliation often become an overwhelming financial and resource burden (amounting to an average of $118 per reworked claim). As a result, nearly 65% of all denied claims are never reworked. The sector is further strained by a 30% nationwide shortage of medical coders.
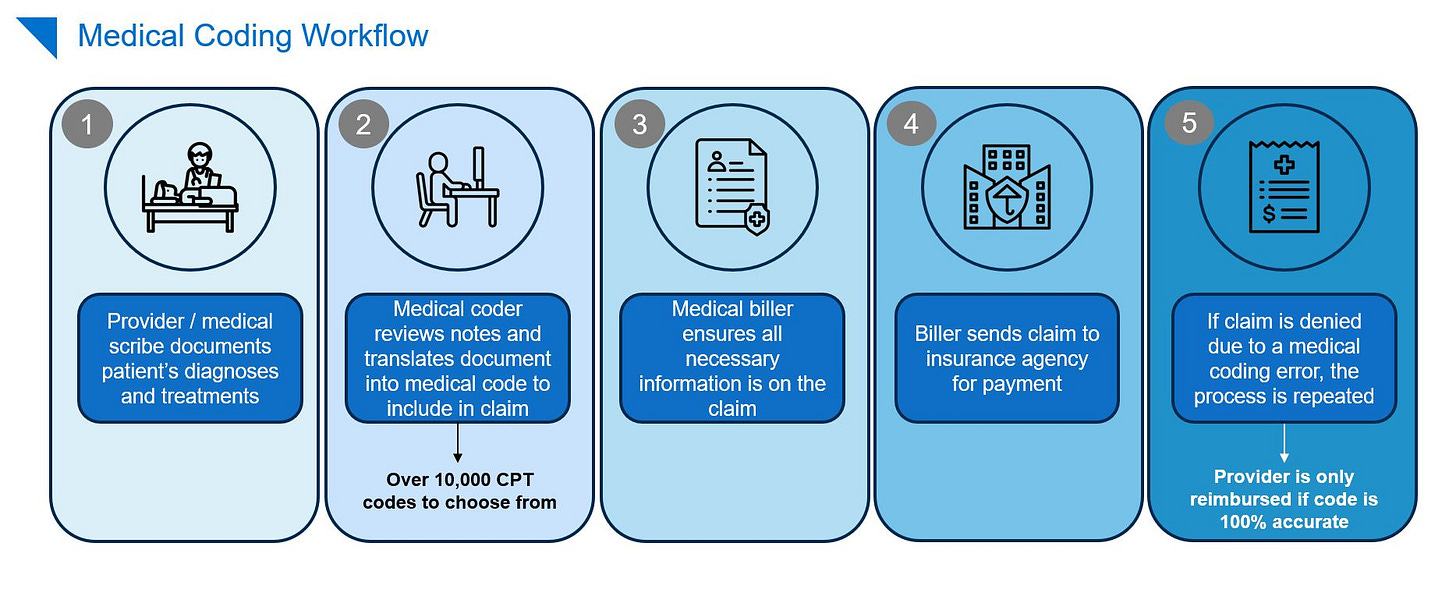
Cue autonomous coding. Groundbreaking AI models can autonomously select the appropriate medical code, requiring human intervention only for low-confidence scenarios. These AI-driven innovations hold the promise of accelerating coding processes while enhancing accuracy — and reducing the massive amount of human capital spent in this part of the revenue cycle management workflow.
Prior Authorization
During a clinical visit, if a physician recommends a specific drug, therapy or procedure, obtaining approval from the patient’s insurance company is often required before proceeding with the treatment. This process is known as prior authorization.
Each health plan has different approval rules and regulations, leading to limited standardization in the process across various health systems. Clinicians and their staff spend an average of 14 hours per week on prior authorization and 35% of physicians have staff who work exclusively on prior authorization.
The prior authorization process can take up to 2 months to complete, and 80% of physicians say that this can lead to treatment abandonment.
If this process could be automated from end-to-end, millions of hours would be saved industry-wide, and patients would be able to access treatments sooner. We see a role for AI in 1) helping clinicians understand the shift nature of what a given payor will cover and 2) draft the request to a payor that incorporates the fullness of the patient record and the relevant medical literature.
On the payor side, an AI-powered tool could help insurance companies respond to provider requests in a timelier manner. For patients, reduced wait time and total rejections will allow for faster access to treatments and care.

Takeaways
We are witnessing the nascent stages of a significant transformation. The early signs of success from players in the space are promising, suggesting that the healthcare ecosystem’s ears are more open than one might think.
We are confident that the next wave of startups will revolutionize healthcare by minimizing costs, reducing administrative burden and enabling clinicians to focus on what matters most—patient care.
If you are building in this space, we’d love to talk.
*Denotes a Battery portfolio company. For a full list of all Battery investments, please click here.
The information contained herein is based solely on the opinions of Brandon Gleklen and Olivia Henkoff and nothing should be construed as investment advice. This material is provided for informational purposes, and it is not, and may not be relied on in any manner as, legal, tax or investment advice or as an offer to sell or a solicitation of an offer to buy an interest in any fund or investment vehicle managed by Battery Ventures or any other Battery entity.
This information covers investment and market activity, industry or sector trends, or other broad-based economic or market conditions and is for educational purposes. The anecdotal examples throughout are intended for an audience of entrepreneurs in their attempt to build their businesses and not recommendations or endorsements of any particular business.
Content obtained from third-party sources, although believed to be reliable, has not been independently verified as to its accuracy or completeness and cannot be guaranteed. Battery Ventures has no obligation to update, modify or amend the content of this post nor notify its readers in the event that any information, opinion, projection, forecast or estimate included, changes or subsequently becomes inaccurate.






